Home / Blog / HRAs for 2020: New choices for small employers, employees
HRAs for 2020: New choices for small employers, employees
Small businesses face unique challenges in employee benefits. Most want to offer the best health care for their employee(s) but must balance that with the realities of the costs of traditional group health plans. Thanks to two new HRAs for 2020, that’s no longer the only option.
An HRA is a Health Reimbursement Arrangement that reimburses the covered employee(s) for eligible out-of-pocket medical expenses. Some plan designs also allow reimbursement of the employee’s health insurance premium. HRAs for 2020 offer employers more benefit choices than ever.
There are two kinds of HRAs for 2020 – stand-alone and GHP-integrated.
Stand-alone HRAs do not require the employer to sponsor a group health plan. The employee selects individual or non-group health coverage (NGHP) on the open market (or ACA marketplace), pays the premium, and then submits receipts for reimbursement through the HRA.
GHP-integrated HRAs are set up to accompany a group health plan. The most popular plan design in this category is the deductible gap HRA, which works with a lower-premium high-deductible health plan (HDHP).
Both stand-alone and integrated HRAs can reimburse for eligible out-of-pocket medical expenses.
Core Documents provides employers with everything they need to establish an IRS- and DOL-compliant Health Reimbursement Arrangement in an affordable, easy-to-use plan document package.
Ready to order? Each section below includes pricing information with a link to our convenient and secure order page for that plan design.
Have questions? Click the contact link to the far right in the blue menu bar at the top of this page or call us at the toll-free number above it.
Stand-alone HRAs for 2020
One-Person HRA Plan
 Coverage for just one employee – sometimes a spouse-employee – a one-person HRA is often the best fit. This type of plan is also known as the Section 105 HRA, in reference to the governing Section of the IRS Code.
Coverage for just one employee – sometimes a spouse-employee – a one-person HRA is often the best fit. This type of plan is also known as the Section 105 HRA, in reference to the governing Section of the IRS Code.
Like any other HRA, the employer determines the amount available to the employee for reimbursement of health insurance premium and related medical expenses during the plan year.
Out-of-pocket expenses eligible for reimbursement with a one-employee HRA include all of those named in IRS Publication 502.
This arrangement provides comprehensive coverage for the employee on a pre-determined budget. It also lets an employee purchasing their own coverage to choose the NGHP that is best for their particular situation.
ACA Coverage Rules
The Affordable Care Act’s (ACA) no annual/lifetime limit and essential health benefits requirement applies to all health plans with 2 or more employees. The one-person HRA remains a viable benefit option exempted from those rules.
⇒
Core 105 plan document package just $199 (.pdf version).
Click to order.
Qualfied Small Employer HRA for > 50 employees
 Employee groups of more than one but fewer than 50 employees are eligible for the Qualified Small Employer HRA (QSEHRA). This plan provides assistance to employees to (1) purchase a qualifying health coverage and (2) pay eligible out-of-pocket medical costs.
Employee groups of more than one but fewer than 50 employees are eligible for the Qualified Small Employer HRA (QSEHRA). This plan provides assistance to employees to (1) purchase a qualifying health coverage and (2) pay eligible out-of-pocket medical costs.
Employer Eligibility
To provide a QSE-HRA to employees:
- The business must qualify as a small employer with fewer than 50 employees, and
- Cannot have any group health plan for any other active employees.
For example, the employer may not offer a QSEHRA to hourly employees while providing a group health plan for salaried workers.
Coverage Amount
The employer determines the amount to provide employees for eligible medical expenses within a plan year (usually on a monthly basis), up to the IRS annual limits:
- The same amount must be provided to all employees;
- The only exception is to have one level for employees with individual coverage and another for those with family coverage.
ACA Coverage Rules
The QSE-HRA differs from the one-person HRA in that the ACA essential health benefits and no annual/lifetime limit rules do apply to the required minimum essential coverage (MEC) for plan participation.
Reimbursement
An employee must purchase MEC on the open market or ACA marketplace and provide proof of MEC before receiving reimbursement for the MEC premium or out-of-pocket medical expenses.
⇒
Core QSE-HRA plan document package just $199 (.pdf version).
Click to order.
NEW in 2020: Individual Coverage HRA for 1+ employees
The Individual Coverage HRA is a new model for plan years beginning January 1, 2020, and later. Like other stand-alone plans, the employer does not provide a traditional group health plan to employees; however, with the ICHRA, an employer may offer a traditional plan to a group of employees that is not offered participation in the HRA.
Employer Eligibility
To provide an ICHRA to employees:
- The church must not offer a choice between the ICHRA and a group health plan to any group of employees.
For example, the company may offer full-time hourly employees an ICHRA while full-time salaried employees are offered a traditional group health plan, but no group of employees may be offered a choice between an ICHRA and a traditional group health plan.
Coverage Amount
The employer determines the amount to provide employees for eligible medical expenses within a plan year (usually on a monthly basis); there is no IRS minimum or maximum limit:
- An ICHRA can be set up to reimburse IC premiums only or to reimburse both IC premiums and other medical expenses;
- The same amount must be provided to all employees in an employee classification group;
- Exceptions can be made within an employee group for employees with dependents and for older employees.
ACA Coverage Rules
The ICHRA must integrate with individual health coverage purchased by the individual on the open market or an exchange.
Reimbursement
Employees must submit proof of individual health coverage at the start of the plan year and with each reimbursement claim.
⇒
Core ICHRA plan document package just $199 (.pdf version).
Click to order.
HRAs for group health plans
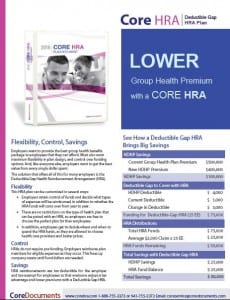
Deductible Gap Plan for 2+ employees with group health insurance
 Reduce the high cost of traditional GHP premiums without putting additional financial burden on employees by integrating a deductible gap HRA with a high-deductible health plan (HDHP).
Reduce the high cost of traditional GHP premiums without putting additional financial burden on employees by integrating a deductible gap HRA with a high-deductible health plan (HDHP).
As its name implies, an HDHP brings with it a higher deductible than traditional health plans. Like any type of insurance, a higher plan deductible brings significantly lower premiums.
To buffer the sting of higher deductibles for employees, an HRA can cover the gap between the former, traditional plan deductible and the increased HDHP deductible.
For example, an HRA covering the gap between a $500 and $1,500 deductible reimburses deductible medical expenses starting at $501 and ending at $1,500 for a total of $1,000 in a plan year. This reduces coverage costs when the $1,000 per year, per employee is lower than the premium savings.
More savings than this is realized, however, because while this coverage is available to every employee covered by the HDHP, it is only actually paid when a deductible medical expense is incurred by an employee. Most employees will have less than the original $500 in deductible expense, meaning they will not draw from the HRA at all.
⇒
Core HRA plan document package just $199 (.pdf version).
Click to order.
NEW: Excepted Benefit HRA
New for 2020 plan years, the EBHRA is available to employers that also offer a traditional group health plan to employees whether the employee chooses to participate in the group plan or not.
Employers may offer up to $1,800 per year to reimburse employees for insurance premiums covering vision, dental, and other medical excepted benefits and related expenses.
⇒
Core EBHRA plan document package just $199 (.pdf version).
Click to order.
Brochures

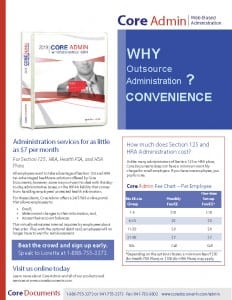
Since 1997, Core Documents has been a leading provider of affordable plan documents required by the IRS, DOL, and ACA for tax-favored employer-sponsored benefit plans, including Section 125 Cafeteria Plans, Health Reimbursement Arrangements and associated flex benefits including the Health FSA, HSA, DCAP FSA, and Transit plans.